|
The following are questions commonly posted on our discussion boards,
along with answers and advice from responding members. In many cases,
member answers have been expanded on from other sources, and relevant
links have been addedfor more information. These answers are meant only
as a helpful guide and a resource for further information; each individual
situation is unique and may need a tailored solution. Your treating psychiatrist
is always a good person to ask when you have specific questions pertaining
to your own case.
If you don't find what you're looking for here, please visit the Schizophrenia
Main Discussion Board (see the righthand menu column on the Schizophrenia.com
homepage ) and post your question. Our members are usually very generous
with their advice and support.
Index of Questions:
Diagnosis and Treatment:
How is schizophrenia diagnosed? How can I tell if
someone has schizophrenia?
What to do if you suspect you or a loved one may have
a psychiatric disorder
What if my family member refuses to see a doctor?
What to do after recieving a diagnosis - how you can help
What is the prognosis? How likely is it that a person
with schizophrenia will ever have a "normal" life?
How is schizophrenia treated?
What to expect after going on medication
What if I can't afford prescription medications?
Working with the psychiatrist
Hospitalization - when and why is it necessary?
The hospital
experience
Choosing a facility
Concerns of families
My son (or daughter) is over the legal age of 18 and the
doctors won't share with me information on his treatment (due to current
laws). What can I do to help my son/daughter, or sister/brother?
How can I help my loved one get the best care
possible?
Why won't my loved one stick to their treatment?
Coping With Schizophrenia:
How do I understand and deal with the symptoms?
(Delusions; Voices/Hallucinations;
Anger/Irritability/Mood swings; Violence
and Abuse; Paranoia; Suicidal
Thoughts and Tendencies; Apathy/Lack of Motivation;
Emotional Flatness and Social Withdrawal)
How Can I Help Someone Who's Depressed?
Why Is Depression So Common Among Schizophrenia Patients?
Possible
causes of depression
How to cope and
where to get help
What are the chances of relapse? How can you plan for
a relapse situation?
How do I explain the illness to family, close friends,
and others?
Living With a Severe Mental Illness - Practical Matters:
Planning for the future - issues for caregivers
and resources to help
Federal Aid and Funding Programs
Health Insurance and Aid
Housing concerns - if your loved one can't live at
home
Job and School Issues - can a person with schizophrenia
go back to work?
How can I help a family member who's been arrested?
How is schizophrenia diagnosed? How can I tell if someone has schizophrenia?
There is currently no physical or lab test that can absolutely diagnose
schizophrenia - a psychiatrist usually comes to the diagnosis based
on clinical symptoms. What physical testing can do is rule out
a lot of other conditions (seizure disorders, metabolic disorders, thyroid
disfunction, brain tumor, street drug use, etc) that sometimes have
similar symptoms.
Current research is evaluating possible physical diagnostic tests (such
as a blood
test for schizophrenia, special
IQ tests for identifying schizophrenia, eye-tracking,
brain
imaging, 'smell
tests', etc), but these are still in trial stages at only a few
universities and companies and are not yet widely used. I t will likely
be a few years before these on the market, and adopted by hospitals,
etc.
People diagnosed with schizophrenia usually experience a combination
of positive
and negative symptoms. These may include (but are not limited to)
racing or uncontrollable thoughts, uncontrollable mannerisms, talking
to yourself, paranoia, hallucinations or delusions, sensing that people
are following or talking to you, insomnia. The Symptoms
and Diagnosis section of this website may help you identify some
of your own symptoms, or the symptoms of someone close to you; however,
only a psychiatrist can make a diagnosis and start a treatment program.
If the symptoms are bothersome, debilitating, or harmful, please make
an appointment with your doctor and/or a psychiatrist.
The best places for schizophrenia diagnosis are the new early psychosis
and schizophrenia diagnosis and treatment centers that are beginning
to be launched worldwide. See our Worldwide
list of early psychosis/schizophrenia diagnosis and treatment clinics
and contact them if you, or someone you know, may be developing schizophrenia.
They have the most intensive testing process and can help get early
treatment (which improves changes of a good outcome).
What to do if you suspect you or a loved one may have a psychiatric
disorder:
The best places for schizophrenia diagnosis are the new early psychosis
and schizophrenia diagnosis and treatment centers that are being offered
worldwide. See our Worldwide
list of early psychosis/schizophrenia diagnosis and treatment clinics
and contact the center closest to you, if you or someone you know, may
be developing schizophrenia. They have the most comprehensive psychiatric
evaluation process and can help get early treatment (which improves
chances of a good outcome).
If you are not close to these early treatment centers or university-associated
psychiatric hospitals (click for list) , then the next thing you
might try is make an appointment with a qualified psychiatrist with
experience with psychosis and schizophrenia. See our section on Finding
and Working with a Psychiatrist (click here) for more information
on how to find a good one.
Another approach is to start with your primary care physician, and
get a full check-up and evaluation to rule out some other common neurological
disorders. Some tests that you might expect include an EEG, MRI, or
PET scan to rule out seizure disorders, and some lab tests to determine
pituitary and thyroid function. The doctor will listen to what you have
to say, hear about what difficulties you're having, and recommend a
course of action. This may be a referral to a psychiatrist. If you are
having trouble finding a good psychiatrist, again see "Finding
and working with the psychiatrist" section of this FAQ guide
for ideas.
It's a good idea to prepare materials and questions to take with you
to your appointments. Keep
a journal of symptoms, odd or troubling behaviors, psychotic episodes,
and anything else that you want your doctor to know about. Make a list
of questions that you want your doctor to answer. "Choosing
the Right Mental Health Therapist" (information provided by
the U.S. organization SAMHSA) has an easy-to-follow procedure list for
appointments, as well as some suggestions for questions you might ask.
What if my family member refuses to see a doctor?
Many people with schizophrenia are literally unable to see that there's
anything abnormal about them (this is commonly called 'lack of insight'
or 'poor insight'). It's almost a hallmark characteristic of the disorder,
like memory loss is for Alzheimer's disease. There are several physical
explanations for impaired awareness - the important thing to realize
is that your relative is most likely not being purposely obstinate,
difficult, or defensive when they deny their symptoms and refuse help.
This, however, leaves you as a concerned family member in an awkward
and extremely frustrating position. Current U.S. laws make it very difficult
to get help for someone who actively refuses it - someone may be actively
psychotic and in desperate straits, but still not considered a serious-enough
threat to themselves or others to merit involuntary hospitalization.
This is a constant source of trouble for families dealing with mental
illness. Visit the Treatment Advocacy Center website to look up state
laws on mental illness
The best course of action depends on the type and severity of symptoms.
If the symptoms are worrisome but not absolutely harmful yet, try locating
a mental health professional or a social worker who is familiar with
dealing with psychiatric disorders. They can discuss your relative's
behavior with you, and brainstorm the best way to get him/her help.
Options will vary from state to state, based on state law. In some areas,
you can call a crisis unit (look in the telephone book or call the hospital)
that will send an evaluation team, and maybe instigate a 72 hour psych
hold. Contact a local NAMI chapter
or call their helpline (1-800-950-NAMI) to look up resources in your
area.
Family members at schizophrenia.com have firsthand experience of what
has worked for them, and what you might do to help your situation. See
their suggestions
and advice on the schizophrenia.com website.
When patients are provided with full and accurate information for understanding
their illness and its treatment, sometimes their insight may improve.
You as a caregiver can play an important role by providing this information,
and presenting it in as optimistically as possible. See 'How
Caregivers Can Help a Relative Accept Their Illness'.
It can be very frightening to go through what your loved one is experiencing,
and a lot of people are hesitant to seek treatment because they are
afraid of being hospitalized. If you can, reassure your loved one that
if treatment is started eary enough, hospitalization is probably not
necessary. Emphasize that medication can make a huge difference in the
way they are feeling.
If the symptoms are very severe, your best option is to persuade a
hospital ER or the police department that your loved one is in grave
danger of harming him/herself or others. Although this might be absolutely
clear to you and other family members, the current strictness of legislation
places a very narrow definition on what counts as "harm to self
or others." Try and become familiar with what the criteria is ahead
of time, so that you can choose the right words to describe the situation.
If the hospital agrees that an involunatry admittance is necessary,
they will begin a three-day (or maybe less, depending on hospital policy)
psych hold. Without a court order, they are not permitted to hold anyone
involuntarily for longer. Talk to the treating physicians about how
to start court proceedings, or see your options for 'Assisted
Treatment' (this can include benevolent coersion, conservatorship
or guardianship, conditional release, outpaitent commitment, or an extended
voluntary commitment).
An Advanced Psychiatric Directive is also an option to discuss during
times when the ill person is in control and in a reasonable frame of
mind. This legal document allows the person with the illness to dictate
what actions should be taken on their behalf (including appointing another
person to make treatment decisions) if they should become unable to
make decisions for their own well-being. Bear in mind that Advance Directives
are not appropriate for all, or maybe even the majority, of people with
schizophrenia. In order for a Directive to be an empowering rather than
a coercive tool, the person who prepares the document for themselves
must have the skills and the social support to make beneficial decisions.
For more information, and for downloadable documents to help prepare
an AD, see the Advanced
Psychiatric Directives section of the Bazelon Mental Health Law
Website.
If the person has EVER violently threatened or actively harmed you,
another person, or themselves, call 911 or an emergency room immediately.
Violence against family members of the mentally ill is a reality, and
you need to protect yourself and everyone by getting your loved one
committed.
What to do after recieving a diagnosis - how you can help:
Whatever diagnosis is given, whether it is schizophrenia or something
else, know that there are many many patients and families out there
with the same questions, concerns, and problems that you face. There
is a wealth of information and support available to you. Here are some
things to try first:
1. Educate yourself and other family members as much as you
can about the illness, the treatments, and long-term prospects. Greater
understanding can help alleviate fears and can make communication, treatment
programs, and day-to-day coping much easier. See
Recommended Books for a list of helpful, reviewed reading material.
There is also a wealth of online information to read here at schizophrenia.com
(where we have over 12,000 pages of information on schizophrenia) and
other websites. Other web sites include that have some good information
include:
NAMI - National Alliance
for the Mentally Ill
MentalHealth.com
- free encyclopedia of mental health information created by Canadian
psychiatrist Dr. Phillip Long.
British
Columbia Schizophrenia Society - excellent resources for family
members
National Institute
of Mental Health - concise overview of different disorders, diagnoses,
treatments, options, and resoureces
Rethink - UK mental
illness charity - wealth of information for patients and family on disorders,
coping, practical matters, etc.
Check out our full list of web-based resources,
including organizations and online reading material
Also check out our online PDF reference library,
with links to the most helpful pdf documents on mental illness and related
issues. Ideal for printing for your own reference files, or passing
out to family/friends/teachers/employers.
2. Watch and Listen to our archives
of internet-based audio and video files on schizophrenia, mental
illness, and related issues. Good files to start with include:
--Schizophrenia Introduction and Overview - An
Educational Video (Schizophrenia Society of Canada)
--Schizophrenia - Second Chances - public radio
program covers the personal experiences of schizophrenia, how to help
people who don't understand they have schizophrenia, and how dramatic
advances in schizophrenia research are providing new hope for people
suffering from the disease.
--Schizophrenia: Treatment, Access, Hope for the
Future? - public radio progam invites a panel of experts to discuss
current research, treatment options, and impact on family members.
3. Build a support network as soon as you can of other families
with similar experiences. The discussion boards at schizophrenia.com
are a good place to start, but a local support group can be a long term
source of relief and resource for you during difficult times. The
National Alliance for the Mentally Ill has local chapters in every
U.S. state - visit their website and find one near you. Also, consider
taking a Family-to-Family class (also through NAMI), a free 12-week
education course designed for (and taught by) family caregivers of people
with severe mental illness. This class is highly recommended by many
members of schizophrenia.com. See the Family-to-Family
website for more program information and class schedules.
4. Find the mental health support resources in your area. Search
a state-by-state
database of available mental health services in the U.S., or try
www.rethink.org for services in the U.K.
What is the prognosis? How likely is it that
a person with schizophrenia will ever have a "normal" life?
With treatment, rehabilitation therapy, and lots of social support
and understanding, many schizophrenia patients can recover to the point
where their symptoms are more or less completely controlled. Many are
living independently, have families and jobs, and lead happy lives.
See the success
stories of some such patients on the schizophrenia.com website.
One schizophrenia.com member had the following to say about living with
schizophrenia:
"Those early years when you are first diagnosed are very
hard. Many people are very surprised by the illness and don't know
what to do. Many refuse medicines. But as time goes on, most people
learn what works. They find their best medication. They find a way
to live that is satisfying and doesn't stress them too much. They
learn not to drink too much alcohol, and to take care of themselves.
The find a good doctor, and often others help them, such as friends,
priest, or counselor. People make a decent life for themselves. They
find love, ,they find work....it gets better. The key is to stick
with the medication, and to never give up."
However, although research has made great strides in both understanding
and treating the disorder, there is still much that we don't know. We
still don't know why some patients deteriorate faster than others, why
some don't respond to medication as well, why some make good recoveries
while others are unable to. It's important to realize that while there
are lots of things that the patient and the family can do to help the
prognosis, schizophrenia is a disease that sometimes takes its own unexpected
course. Setbacks are to be expected, and are not signs of failure on
anyone's part. It's important to set your own expectations and goals
(whether you are the person suffering from schizophrenia or a caregiver)
to an achievable level, and appreciate accomplishments for what they
are rather than what they're not. One schizophrenia.com member pointed
out that everyone's "climbing the ladder" of life, but someone
who starts from the bottom and manages to climb up halfway has achieved
a lot more than someone who starts at halfway but only climbs a rung
or two.
There are factors in the course of the disease that can, to a certain
degree, help predict the various outcomes. You can improve the chances
for a good prognosis by knowing
what the indicators for possible relapse are, working to get the
best possible treatment as quickly as possible, and learning how to
effectively self-manage a long-term mental illness. The mentalhealth.com
website also has information on what
family members can do to help ensure the best possible outcome.
For a good presentation on the prognosis for people who have schizophrenia,
and an update on new treatments for schizophrenia see the Stanford
University "New Treatments for Schizophrenia" presentation.
How is schizophrenia treated?
American Psychiatric Association's
Guideline For The Treatment Of Patients With Schizophrenia states:
"antipsychotic medications are indicated for nearly all acute psychotic
episodes in patients with schizophrenia." In addition to antipsychotic
medications, some patients also take anti-depressants or mood-stabilizers
to help control related symptoms.
Medications work successfully in the majority of patients (approximately
70% of patients will improve, according to research - but we've also
seen research that suggests the chances of any one drug working for
a person may be only 50% so people frequently have to try more than
one drug to partially or completely control the positive symptoms (hallucinations,
delusions, paranoia, racing thoughts, etc). They are not as effective
in controlling negative symptoms, and may cause side-effects of their
own. See our Medications
area for information on commonly prescribed antipsychotic medications
- how they work, how effective they are, what side-effects they cause
- as well as additional info on research studies and medications in
clinical trials. See also New
and Newer Mechanisms of Action for Antipsychotic Medications, an
online UCLA grand rounds video presentation that explains (in some detail)
what areas of the brain different drugs target, and what effects they
have.
For a good presentation on the prognosis for people who have schizophrenia,
and an update on new treatments for schizophrenia see the Stanford
University "New Treatments for Schizophrenia" presentation.
Although an important element, medication is far from the only treatment
used for schizophrenia patients. Many patients and their families choose
supplemental therapies (these can include psychosocial or cognitive
therapy, rehabilitation day programs, peer support groups, nutritional
supplements, etc) to use in conjunction with their medications. In certain
severe cases, some patients also respond to electroconvulsive
therapy (which has been shown to be safe and effective) or transcranial
magnetic stimulation (TMS).
In the case of therapy, some research has shown that psychotherapy
and medication can be more effective than medication alone (however,
the same study noted that psycotherapy alone was NOT a substitute for
medication). The three main types of psychosocial therapy are: behavioral
therapy (focuses on current behaviors) cognitive therapy (focuses on
thoughts and thinking patterns) and interpersonal therapy (focuses on
current relationships). For schizophrenia, cognitive-behavioral therapy
has shown the most promise in conjunction with medication.
For some supplementary treatments options (as well as "alternative
therapies" that have been disproved), see Other
Treatments on the schizophrenia.com homepage.
For more information, see Treating Schizophrenia - What Are the
Options? (ABC News webcast). ABC news host talks with a panel of
experts about what treatments are out there and how successful they
are.. Link
to video file and transcript. (If
you don't have it, Download Quicktime video player.)
What to expect after going on medication:
Medication can greatly decrease symptoms and help a person return to
a functional level; however, every case is unique, and medications are
not perfect. It will likely take a long, frustrating trial-and-error
process before a treatment regimen is found that works best for the
patient.
When a psychiatrist prescribes any medication, ask what symptoms it
primarily treats, what the common side effects are, what dosage he/she
is prescribing, and how long it will take to start working. Keep track
of every medication (and at what dosage) you (or your loved one) is
on, what side effects it causes, which symptoms get better and which
get worse. A journal (the same journal where you write down symptoms
and behaviors) is an excellent place to do this.
Don't be surprised if the doctor keeps switching medications, or adjusting
dosages. They are not frivolously experimenting; trial-and-error is
the only way to eventually find a combination that works. Medications
are never a perfect fit: a prescription can work for awhile and then
stop working, or one that you tried previously may work at some point
in the future. You can help this process with feedback about the different
medications (see paragraph above).
An antipsychotic medication can take weeks or even months to start
working at full strength, so be patient and keep recording things in
your journal. Medications are less likely to make any huge, noticeable
changes in life; instead they should make things generally "easier."
Once you find a medication that seems to work, the voices/hallucinations
may gradually fade away and disappear - or they may not. Sometimes these
voices quiet down to a point where they are not harmful or debilitating,
and many people with schizophrenia make a decision at this point that
living with these quieter voices in the background is preferable to
going through the pain of more medication and more side-effects.
Some general things to be aware of:
Both the illness itself and many of the medications used to treat it
can make a person feel overly tired or lethargic. You may need to sleep
more than you think, and it may be unrealistic to try and dive head-on
back into your normal activities. Recovering from schizophrenia is like
recovering from any long-term illness. Plan small goals to ease yourself
back into a routine that you enjoy, and don't expect too much of yourself
at first in terms of socializing. Be aware if others are pushing you
too hard to "get back out there" - give yourself the time
and support you need.
What if I can't afford prescription medications?
Without a good health insurance plan, antipsychotic medications (particularly
the newer ones) can be terribly expensive. However, you have some options
even if you are currently unemployed or uninsured. Here are a few suggestions:
- Apply for Supplemental Security Income (SSI) or disability benefits,
federal funds that are available for physically or mentally disabled
persons who are unable to work. See Schizophrenia.com's Help
with SSI page, or the Social Security
Association website for more info on programs and how to apply.
- See if you qualify for Medicare (for elderly) or Medicaid (for low
income persons) health coverage. Your doctor or a hospital social worker
can advise you on your eligibility, and help you apply. See also
"Living With Schizophrenia - Practical Matters" in this
FAQ guide for a list of federal aid programs for disabled or low income
persons.
- The older antipsychotics tend to be cheaper than the newer ones -
discuss with your doctor the possibility of using a cheaper alternative.
Be aware, though, that the older medications also may have significantly
more side-effects, and are not as effective controlling negative symptoms
- Information
on available low-cost medications, and what benefits are available
to mentally ill or disabled persons, is available on the schizophrenia.com
website
Finding and Working with the psychiatrist:
A good psychiatrist can and should be an ally in the continual process
of treatment and recovery. They should be willing to work with you as
an informed member of the treatment team and ideally they should be
well-informed and experienced in treating schizophrenia and related
disorders. Here are some suggestions to help you find a psychiatrist
you can effectively work with:
Hospitalization - when and why is it necessary?
At some point or another, most people with schizophrenia will likely
have to be hospitalized for at least a short time. Hospitalization can
be voluntary (requested by the patient themselves) or involuntary, meaning
it is up to the discretion of the treating psychiatrist, emergency room
staff, or a courtroom (see
the criteria and procedures for involuntary hospitalization by U.S.
state). At the point of hospitalization, a person may be in pretty
bad shape - feeling sick, scared, out of control, and abandoned. Understandably,
at the time it's not a pleasant experience for anyone involved. But
it doesn't have to be something to fear.
Why might somebody need hospitalization, rather than outpatient
care?
- patient needs to be in a protected environment to keep them from
harming themselves or others.
- patient needs to be monitored by trained professionals for symptoms
and medication reactions.
- patient needs a safe place where they can stabilize and concentrate
on recovery.
- family needs a short respite to gather themselves and make long-term
treatment plans.
What can you get with hospital treatment that you can't get as an
outpatient?
- constant monitoring in a controlled setting, so medications can
be adjusted more quickly and accurately. Hopefully, this means you
start feeling better sooner.
- more time with a doctor and/or therapist, maybe every day. Trained
staff members are always around to talk to about questions, concerns,
or thoughts.
- group therapy, recreation programs, vocational/social rehab (programs
will vary depending on the hospital)
- A safe place to gather yourself, get settled with medication, and
stabilize so you can return to your own life as soon as possible.
- according to one schizophrenia.com member: "plenty of rest,
free food, free laundry, you get to meet nice people, free recreation,
[and] you get a chance to draw pictures and watch a show or two."
Many members of schizophrenia.com have written
about their experiences in hospitals (either voluntary or involuntary)
on the discussion boards. Most agree, at least in retrospect, that getting
treated in the hospital was the best thing for their health and well-being
at the time. Some of their thoughts are quoted below:
"It's nothing to be scared about. Try the meds they give
you and work with the staff. They are there to help and want you to
talk to them when you are having problems. The other patients on the
ward will have different illnesses than just schizophrenia, like bi-polar,
depression and drug addiction...Hopefully if you go you can get things
straighten out."
"I found that I was at my worst the two times I was at the
hospital. So I did not like being there at all. But it was a place
where I was safe, a place where I couldn't hurt myself or wander off.
The hospital is the place my healing started, and I find that it was
not an enjoyable experience but a helpful one."
"[T]he better your attitude about being hospitalized and
the more hope you have for yourself, the better you will do, I think.
I had faith that the medicine would help me from the beginning, and
it turned out to be true."
"[S]ometimes, as my pdocs have said over the years, we need
a "safe place" and sometimes that is the hospital."
Once it has been determined that hospitalization
is necessary, you may have a choice (depending on insurance, availability,
and your psychiatrist's recommendations) of what hospital to go to.
Psychiatric facilities include public hospitals (state, county, or community),
university (teaching) hospitals, private psychiatric treatment centers,
and VA hospitals. Dr. E. Fuller Torrey, in his book "Surviving
Schizophrenia" (pp. 180-188)offers the following suggestions
for evaluating psychiatric in-patient facilities:
- talk to your doctor, treating psychiatrist, hospital staff, and
other families who are familiar with programs in the area; ask for
their recommendations and reviews of various programs
- look for a Joint Commission on Accreditation of Health Care Organizations
(JCAHO) accreditation. A JCAHO team, upon invitation by the hospital,
surveys patient care and services, therapeutic environment, safety
of the patient, and quality of staff and administration. The hospital
may receive full 3-year accreditation, full accreditation with a contingency
(meaning that a follow-up inspection may be warranted), or no accreditation.
Bear in mind that accreditation is given to hospital as a whole,
NOT to individual wards. Ask for JCAHO accreditation at the hospital
administration office, or look for a certificate by the entryway or
in the lobby.
- the quality of staff, first and foremost, should indicate the quality
of the ward. Due to the staff, even individual wards in the same treament
facility may vary in quality.
- do NOT assess quality by fees charged. Private facilities are not
necessarily better than public ones. Again, evaulations of the staff
at each location should guide you.
Hospitalization is no easy experience for friends
or family members either. Especially if commitment was involuntary,
family may be hesitant about visiting, unsure of how to react when their
loved one returns home, and fearful that their loved one will never
forgive them for making that hard choice. One schizophrenia.com member
had the following thoughts about committing her child:
"In the early years, I would grieve myself so badly I would
get physically sick. I felt so much guilt if I allowed myself the
slightest amount of pleasure, so instead would stay in continuous
grief mode. It consumed me day and night - all I could think of was,
what was what my child going through at that very moment? What kind
of a Mother could I be if I dared allow myself to read a book, go
to a movie, etc. when my son was locked up...
This I tell you serves no purpose. You need to be kind to yourself
right now. Enjoying a bubble bath, going window shopping, having a
laugh, does not mean you do not care and are not concerned. Instead
it enables you to focus on helping your child and keeping up your
spirits so you can show them a positive attitude."
Keeping a positive attitude, even through the difficult experience
of hospitalization, is something that many family members stressed as
important. As one relative said, "It's so important to be cheery
& positive when you visit them in hospital. I found it helped a
lot if I just talked as if I EXPECTED him to be better soon."
Some family members are unsure about visiting, not knowing what to say
or if their loved one even wants to see them. Visiting might indeed
be difficult until medications start working - the ill person is not
feeling well, and may be angry, frightened, or even out-of-control.
In retrospect, most people who were committed agree that they needed
to be hospitalized at the time, and appreciate that someone was looking
out for them. Even if your loved one refuses to see you, or is angry
with you, showing your love and support by continuing to go is one of
the best things you can do. It helps to get through to them, even subconsciously,
that they have not been abandoned. Below are thoguhts on visiting from
schizophrenia.com parents:
"He hated us for putting him in there.... until the meds
kicked in. (He was never happy we did it, but never held a grudge
that we did.) We went each evening after work all the way to the hospital
to see if he would visit with us. The answer was always no, so we'd
turn around and head for home. But we went anyway. The reason? Because
we felt (and so did the psychiatrist we had then) that deep inside
that pile of rage and paranoia was our son. And that deep down inside
he needed to know that he was loved. So we went, were turned away,
and did the same the next day or so, until the meds had kicked in
and he wanted to see us."
Other things family members can do to make the hospital stay as easy
as possible:
- Get to know the ward staff, so they know that someone is actively
interested in the welfare of that particular patient. These are also
the people who will ultimately be able to explain to you what is going
on with your loved one, and help address your questions and concerns.
- Arrange for a tour of the facility, and become familiar with admissions
procedure, daily schedules, and visiting hours and regulations.
- Ask about any rules regarding bringing a patient gifts, photographs,
or food.
- Ask to be notified when your loved one is getting ready to be discharged.
- Learn about the treatment plan, and find out what your role in it
can be.
- Talk with the staff before your loved one is discharged about how
to continue care at home, what signs might signal a relapse or a mdeication
reaction, and how to make the transition to living at home as smooth
as possible for everyone.
The following online resources have more information about the logistics
and experience of psychiatric hospitalization:
--involuntary commitment
- another section of the FAQs, deals with procedures for commitment
and common fears/concerns of loved ones making the decision.
--Let's
Talk Facts about Psychiatric Hospitalization (APA publication).
--Psychiatric
Inpatient Experiences - a personal voice on what psychiatric hospitalization
is like, and advice to make it a more positive experience.
--a public radio show about
mental hospitals (particularly Bellvue in New York)
--Psychiatric Hospitalization:
What It's Like on the Inside (radio program)
--Returning
Home - an online booklet for families about helping a loved one
transition back into the home environment after spending time in a psychiatric
facility.
My son/daughter or brother/sister is over the
legal age of 18 and the doctors won't share with me information on his
treatment (due to current laws). How can I make sure my son/daughter is
getting the best possible treatment and the doctor is well informed?
While doctors and nurses "BY LAW" are not allowed to talk to
you about the situation with your son/daughter or brother/sister if they
are over the age of 18 (in most states). Many doctors and nurses are sympathetic
to the challenges the family faces - but they have to follow the law or
they could lose their jobs.
The doctors are, in most situations, required by Law to tell the patient
if they talk with you, and generally cannot talk with you - but the tip
here is that a lot of smarter and more compasionate doctors know of the
challenges that families face and so "bend" the rules a bit.
In a recent presentation by a psychiatry doctor at one of the top medical
schools in the US said that what she would do is accept phone calls from
family members and let them talk to the doctor (her) - and listen to the
family member (for example to let the family member tell the doctor of
what the behavior was at home recently, the delusions, actions, etc. -
for example if the ill family member is in the hospital for a 72 hour
hold and the hold is about to expire - but the doctor would not "speak"
back to the family member who was calling - just listen. This woman said
that if she got such a phone call she would quickly add another 72 hours
to the hospital "hold" to help give the ill person time to start
working towards recovery.
So - if you call the doctor, and tell them that you know that they can't
talk to you - but if they just hold on to the phone so that you can tell
them some things, that you don't think that this would be breaking the
rule of patient confidentiality...
Of course - every doctor is different.
If the behavior of the family member is potentially violent or dangerous
and the hospital or doctor is not being responsive in a way that you think
is best for your son or daughter (or sister or brother) then you may have
to let the doctor and hospital know (in writing) that you will hold them
legally liable for anything that happens because they are not doing their
job and treating the mentally ill person. See: How
to Force the System to Give You or Your Family Member Better Care
for more information.
And yes - in our view its a very stupid law that prevents a parent from
helping and being involved in their mentally ill son's or daughter's treatment;
its a legal response designed for situations where the person is mentally
capable, not mentally ill. These laws make it very difficult to get help
for your mentally ill family member, and difficult to understand how to
best help the mentally ill family member (who is frequently living in
the same house!). You can work to change the system to make it easier
for families to get treatment for the people who need it - by contacting
the organization called the Treatment
Advocacy Center.
How can I help my loved one get the best care possible?
It can be frustrating working within the modern healthcare system.
Especially in the middle of a crisis situation, when everyone is stressed
and frightened, it can seem like no one is paying attention to your
or your loved one's needs. However, there are many things you can do
to communicate effectively and get the care you need and deserve. Here
are some resources to help:
1) Make sure the doctor/psychiatrist is aware of all the symptoms -
if they don't have all the information, they might be led to an incorrect
diagnosis. Keeping a
symptom journal is the most thorough and accurate way to do this.
2) Become familiar with the treating psychiatrist, the nurses at the
hospital, the social workers, and anyone else directly involved with
your relative's care. These are the people who should have your loved
one's best interests and welfare at heart, and the people you should
go to if you have questions, concerns, or complaints. Be assertive -
you have every right to know what is going on, and have things explained
to you in a way you understand - but be polite and flexible also. Too
many times hospital staff get impatient with "problem" family
members who they see as rude or demanding. It's vital to have a good
working relationship with the treatment team.
3) Be polite but persistant in your quest to get information and answers.
Hospital staff members are inevitably busy, but they are there to give
the best care possible to consumers and their family. Keep your conversations
and requests short and to the point, to maximize the time they have
for you. If they are unable to see you, leave a message with your name,
your relative's name, and your number, and keep the phone line clear
so they can reach you at the first opportunity. Consider putting your
question or request in a letter, and delivering it to their office.
Remember to write down things you appreciate - special considerations
or care that you or your relative recieved from a care provider - as
well as concerns.
4) If you are an immediate relative or caretaker, make sure that you
have clearance to speak with the psychiatrist and other doctors about
the diagnosis and treatment plans. Current confidentiality laws prevent
doctors from speaking with anyone other than the patient (assuming the
patient is a legal adult), unless the patient gives their official permission
with a HIPPA (Health Insurance Portability and Accountability Act) compliancy
form. It can be absolutely essential for another person (a family member,
primary caretaker, etc) to be informed of treatment decisions, especially
because so many people with schizophrenia have very little insight into
their own illness. Getting confidentiality clearance ahead of time can
prevent many battles in the future over treatment compliance. See 'Involvement
of Family Members in Treatment Plans for their Hospitalized Relative'
for more ideas.
5) See 'How
to Get Better Care' for ideas on how
to work cooperatively with the hospital staff and the treating doctors
to improve care.
Why won't my loved one stick to their
treatment? How can I convince them to take their medication without upsetting
them, or making them feel like I'm the enemy?
According to schizophrenia expert Dr. E. Fuller Torrey ("Surviving
Schizophrenia" 4th ed, p. 295), there are several reasons that
people with mental illnesses refuse or stop treatment (also known as
"medication noncompliance). These reasons include:
- Lack of insight into the illness (also called anosognosia - a biological
symptom of the disease)
- Denial (a psychological issue - person is aware of illness but wishes
not to be ill)
- Medication side-effects
- Poor doctor-patient relationship
- Delusional beliefs about medication (e.g., that it is poison)
- Cognitive deficits, confusion, disorganization
- Fears of becoming medication-dependent or addicted
Some of these reasons are easier to deal with than others; for example,
you always have the option of finding a better doctor, or adjusting
medications to reduce side effects. Providing the patient with information
about their illness (the benefits of medication, the long-term prognosis,
etc) has been shown to improve compliance.
Simplifying the treatment regimen with single daily doses, use of compartmentalized
pill containers, long-acting injections, etc. can also help.
Unfortunately, one of the most difficult reasons for medication noncompliance
is also one of the most common - statistics estimate that 40% of schizophrenia
patients lack insight into their own illness as a symptom of the disease.
Such anosognosia makes an enemy of anyone who tries to convince them
otherwise. There is sometimes no way to force compliance without long
and upsetting battles with your loved one. However, medication is currently
the best tool we have to control psychotic symptoms and improve patient
insight. Many members of schizophrenia.com have indicated on the discussion
boards that living with schizophrenia is difficult enough with
medication; without it, it's downright impossible.
You do have options available to you. Assisted Treatment is a benign
term for an extremely difficult task - to help (or 'assist') a loved
one with their treatment because they are unwilling or unable to take
care of themselves. Assisted treatment options may include benevolent
coercion, obtaining conservatorship or guardianship, conditional release,
outpatient commitment, or involuntary commitment. The Treatment Advocacy
Center website has excellent information
and resources on Assisted Treatment.
A less extreme technique suggested by other schizophrenia.com members
is to ask your loved one to try the medication for a specific period
of time. Hopefully, once the medication starts to take effect, the person
will begin to regain some rational thinking skills, and you start to
talk reasonably together about the benefits of long-term treatment.
However, make sure you give the medication enough time to work - it
can be at least 1-2 weeks before any improvement is noticed, and many
antipsychotic medications don't take full effect for weeks or months.
Others at schizophrenia.com have come to the extremely difficult point
of offering their loved one an ultimatum - either get treatment and
stay med compliant, or someone is going to leave (either you, or the
patient). Another similar method of coercion is to stop supporting your
relative financially unless they agree to treatment. There is no way
to know or guarantee the results of such an ultimatum, so consider carefully
if you are willing and able to follow through with your threat. It will
only work if you are committed to carrying out your words. Also consider
carefully your own safety and the safety of your family before making
such a threat, since the illness can make some people behave unpredictably
or violently, even against someone they love.
For more ideas and resources for dealing with the difficult subject
of treatment compliance, see the following:
Coping With Schizophrenia:
How do I understand and deal with the symptoms?
Each case of schizophrenia will have a unique combination (in terms
of severity, duration, prominence, etc) of positive, negative, and other
symptoms. Related conditions such as depression, anxiety disorders,
and mood-swings are not uncommon either.
One schizophrenia.com member diagnosed with the disease described his
symptom experience with the following words:
The things that I have that I wish I didn't have are hallucinations,
delusions, and loss of thought control.
The things that I don't have that I wish I did have are curiosity,
motivation, and sex interest.
The above is pretty much the way schizophrenia goes.
Many family members struggle to understand what their loved one is
dealing with, and want to relate and empathize with their illness experience.
One of the best ways to understand what is behind some of the common
symptoms of schizophrenia is to educate yourself as much as you can.
"Surviving Schizophrenia" (Dr. E. Fuller Torrey) and "I
Am Not Sick! I Don't Need Help! (Xavier Amados) are two books repeatedly
recommended by veteran families on schizophrenia.com for people searching
to better understand the experience of mental illness. Other
recommended books, videos, and websites can be found on the schizophrenia.com
website.
Some general materials to help you live and cope with the symptoms
of someone diagnosed with schizophrenia include:
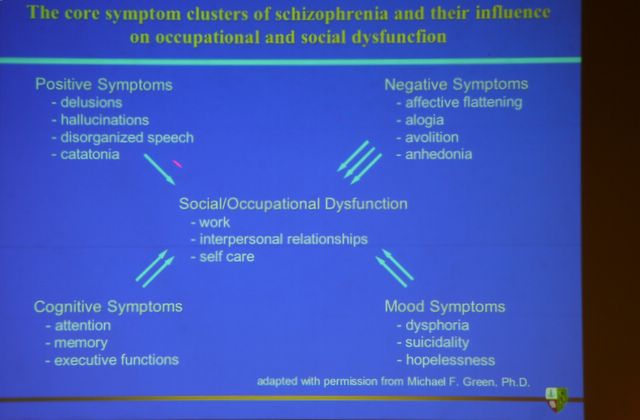
Source: Presentation
by Dr. Ira Glick,"New Schizophrenia Treatments" - Stanford
University Schizophrenia and Bipolar Education Day, July 2005
(Click to see full presentation) Explanation of Terms:
Delusions are fixed inaccurate beliefs, hallucinations are seeing or
hearing things that are not actually there, Catatonia is an abnormal
condition variously characterized by stupor, stereotypy, mania, and
either rigidity or extreme flexibility of the limbs, Affective Flattening
means that a person with schizophrenia will tend to have a flat emotion,
or be emotionless much of the time, Alogia
is the inability to speak, Avolition is a lack of motivation or desire,
Anhedonia
is the inability to experience pleasure. Dysphoria is
an emotional state characterized by anxiety, depression, or unease.
Executive functions are the brain's thought processing abilities that
allow people to plan and problem solve (and which are typically significantly
decreased by schizophrenia).
The following are specific suggestions that schizophrenia.com members
have posted on the discussion boards concerning some common symptoms
of schizophrenia and their associated problems.
Delusions: The common categories
of schizophrenia delusions include persecution delusions (feelings that
you are being spied on, conspired against, cheated, drugged, or poisoned),
jealousy delusions (a feeling without just cause that your loved on
is unfaithful), and self-importance delusions (also known as delusions
of grandeur - the feeling that one has a great but unrecognized ability
or talent, or the belief that you are an exalted being. Sometimes these
have a religious flavor to them). It's upsetting and frustrating (to
put it mildly) to be the victim of such delusions, especially when your
only goal is to love and support your ill relative; however, the closest
family members and relatives are often the first targets of this and
other hurtful behavior.
Due to the disease, a person with schizophrenia often can't think or
reason rationally. Explaining logically why the accusation can't be
true won't work, and will ultimately be draining and frustrating, due
to this fact. Try talking directly with the psychiatrist about the delusional
symptoms - the current medication may not be adequate to control them.
Also, be aware that delusions can take weeks or months to fade, even
if the person is medication compliant.
Voices/Hallucinations: The experience of
hearing voices or seeing visions are as real as anything else to the
person with schizophrenia. Like delusions, it usually does no good to
try and refute them. On the other hand, it's also not a good idea to
just "go along with them," which ultimately doesn't help anyone.
Family members who have tried to support their loved ones in the search
for "them", or tried to keep "them" out with elaborate
security devices, have only ended up frustrated. There are no lock to
keep out invaders in your mind; no matter how hard you search, "they"
will always be there.
One thing you can do is to simply acknowledge that your loved one is
experiencing something unique to them - you can say "I'm sorry
it's bothering you" or "why don't you tell the doctor about
it," which doesn't ignore their experience but also doesn't give
false evidence that others can see or hear these things. Sometimes the
best thing that family members can do is encourage the ill person to
write down/remember their experiences, and discuss them with their doctor.
Anger/Irritability/Mood Swings: Try to steel
yourself internally; recognize that this is the illness talking, not
the person. Some people have tried a detached, non-reaction to their
relatives' anger; others have waited for the episode to pass (or calmed
themselves down by going for a short walk) and then communicated how
much they were hurt by that behavior. If mood swings are severe, a mood
stabilizer might be beneficial. Talk to the doctor about possible options.
Violence or Abuse: Call 911 or the emergency
room and get help. Your first obligation is to yourself, your own safety,
and the safety of other family members. If you truly feel that you are
in danger, if you have ever been hurt or seriously threatened, convince
the authorities any way you can of the seriousness of your situation.
Do not accept a diagnosis of schizophrenia (or anything else) as an
excuse for this kind of harmful behavior. The disease may affect a person's
thoughts and perceptions, but abuse is still abuse. What you need is
not just action for domestic abuse, but an involuntary commitment to
a treatment center and a psych evaluation.
Paranoia: See 'How
to Manage 5 Common Symptoms of Schizophrenia', which has 6 steps
for dealing with paranoia. Try to know and avoid situations that overstimulate
or ovewhelm the person - too much sensory input at once can contribute
to paranoid or delusionary symptoms.
Suicidal Thoughts and Tendencies: Suicide
is a real and tragic consequence for many schizophrenia patients - about
40% will make at least on attempt, and between 10% and 15% actually
succeed in killing themselves. A major factor is depression, which is
a common companion of schizophrenia disorders. See 'Managing
Depression' for further information on this topic, or the section
on depression further down in this FAQ guide. If your loved one seems
depressed, you can ask the psychiatrist about the possibility of taking
an antidepressent medication in addition to antipsychotics.
Family and friends can help by being very aware of depressive and suicidal
tendencies, especially in those individuals recently recovering from
an episode or a relapse. See 'Preventing
Suicide' for warning signs and actions that you can take to prevent
a tragedy. If
you are currently thinking about suicide, please read this first.
Know the places you can call on quickly for help - find the crisis centers
in your area and know the services they provide. Contact local NAMI
chapter and ask them about such services.
Apathy/lack of motivation: Although many
people believe that these sorts of behaviors are due to medication side
effects or a lack of will on the part of the patient, most often they
are simply another symptom of the disorder. (Excessive apathy - i.e.
sleeping all day - may be a medication side effect that is compounding
the disease symptom. Talk to the psychiatrist about the possibility
of adjusting meds). The current generation of antipsychotic medications
are much better at treating the positive (psychotic) symptoms, but have
not made major headway against the more cognitive/behavioral negative
symptoms. When you consider that schizophrenia severely disorders the
way an affected individual senses and perceives the world, it's easier
to see why that person might stridently avoid any sort of stimulation,
even just going out to a mall or riding on a bus. One schizophrenia.com
member suggested a comparable situation: two guys are climbing a mountain,
but one is carrying a backpack full of tennis balls and one is carrying
a backpack full of rocks. It may seem that the one is lazier for not
going at the same pace, but he's got a heavier burden to carry.
One of the best ways to help is to actively pay attention to your loved
one's responses. If they respond positively to your overtures or your
attempts at conversation, by all means continue. If you feel rejected
or rebuffed, remember that it is most likely a protective mechanism
against too much sensory overload; stop and try again later. Establishing
small routines or rituals can be very helpful, and a good source of
shared time.
Emotional flatness or social withdrawal: Many
family members are hurt by a feeling that their loved one is emotionally
withdrawing into themselves, and that they just don't relate or interact
anymore to the people around them. Emotional withdrawal/flatness is
one of the negative symptoms of schizophrenia. Some of the newer antipsychotic
medications can help alleviate these negative symptoms; however, they
are not 100% successful, and the response is different from every patient.
One member described his emotional responses in the following way:
"As a schizophrenic I will tell you that my emotions are not just
hard for the world to access, sometimes it is also hard for me to access
my own emotions."
Schizophrenia patients often have trouble with common social cues that
most people do and recognize without thinking - body language, eye-contact,
gesturing, varying the tone of the voice, etc. They don't realize they
are missing these basic cues, and their absence can make the person
seem much more withdrawn and cold than they intend to be. 'Coping
with schizophrenia: social deficits' from mentalhealth.com has good
explanations and suggestions for dealing with this.
Experienced members suggest finding other emotional outlets for yourself
- make time to go out with other friends or just you, and spend another
time with your loved one. Another thing you can do is specifically bring
to the person's attention the fact that you want to share something
with them. Sometimes you may have to simply, lovingly, request their
love and attention.
How Can I Help Someone Who's Depressed? How
Common Is Depression in Schizophrenia Patients?
According to the president of the 20th Collegium Internationale Neuropsychopharmacologicum
(CINP), comorbid mood disorders (such as depression) are so prevalent
in this patient group that they may be considered a fundamental characteristic
of schizophrenic disorders. Up to 80% of schizophrenia patients experience
serious depressive symptoms.
There are several reasons why a person with
schizophrenia is more likely to experience depression than the average
person. Depression may be a biological symptom of the disease - one
of the negative-category symptoms like apathy. This can be compounded
by the extra burden of stress carried by someone living with a chronic
disease. Depression or mood-blunting might be a side-effect of an antipsychotic
medication (abilify and risperidol are two that schizophrenia.com members
have indicated can cause depression). Depression might be a co-diagnosis
along with schizophrenia - some of the same neurotransmitter imbalances
that are implicated in schizophrenia may also contribute to the development
of depression. Finally, depression may be the major diagnosis - for
example, if a person has manic depression, or major depression with
psychotic features. These patients still experience hallucinations and
delusions; however, they tend to have a characteristically negative
tone (for example, a person might believe he/she will cause the world
to end, or he/she is guilty of some unforgivable crime).
Likewise, depressive symptoms can appear at various points during the
course of the illness. Many patients who experienced depression before
starting on a treatment program reported that their depressive symptoms
initially faded with the start of antipsychotic treatments, but then
returned once the positive symptoms stabilized. There could be both
a biochemical and a psychological factor to this. As visions of grandeur
and self-importance, ideas of divine missions, and voices that have
been constant companions for years begin to slip away, many people understandably
feel lonely and isolated. They are frightened as they wake up to a new
"real" world that is unfamiliar and difficult to navigate.
Says Dr. Wingerson (psychiatrist) in Rosalynn Carter's book 'Helping
Someone with Mental Illness': "To be psychosis free with nothing
to look forward to can be devastating" (p. 141).
Regardless of the cause, depression is important
to treat, especially given the high rate of suicide among schizophrenia
patients. Moreover, research has indicated that depression has a profound
effect on quality of life, irresepective of the presence of other schizophrenia
symptoms. "Quality of life among people with schizophrenia may
be more closely related to levels of anxiety and depression than to
the core symptoms of the disorder such as hallucinations, delusions,
and anhedonia" ("Quality
of life in schizophrenia: contributions of anxiety and depression."
Schizophrenia Research, 2001:51(2-3):171-180).
Schizophrenia.com members suggest the following to help deal with depression:
- write your feelings/thoughts in a journal to share with your psychiatrist
or a family members/friends, so someone knows how you are feeling
on a daily basis
- try not to isolate yourself. If you're not feeling up to socializing
or talking face-to-face, a good alternative can be reaching out through
emails, chatrooms, and discussion boards. Many members say that peer
support groups are invaluable to them.
Says on member, "I was an isolationist for a long time, and it
only contributed to the depression and negative symptoms I experienced.
You need to have someone you can talk to, whether it's through a support
group, friends, or an online forum."
- ask your psychiatrist about starting an antidepressant medication.
Many schizophrenia patients take an antidepressant in addition to
anti-psychotic meds. Common options include: SSRI medications (Prozac,
Celexa, Paxil, Zoloft, Lexapro), Effexor, Venlafaxine, Wellbutrin.
Remember to give the meds a month or two to take full effect - see
"What
to Do for 6 Weeks While you Wait for Antidepressants to Kick In"
for coping strategies in the meantime. Also, be aware that your body
might get "accustomed" to the medication. Let your psychiatrist
know if depressive symptoms return, so you can get your medication
adjusted or changed.
- Psychotherapy is one of the cornerstones (along with medication)
for schizophrenia and depression treatment. It helps improve day-to-day
functioning, social skills, quality of life, and motivation at the
same time that medication is improving chemical balances in the brain.
Moreover, studies have shown that psychotherapy causes similar alterations
in brain function to those seen with medication, although it only
seems to be effective in conjuction with medication therapy.
- Nutritional supplements have been shown to increase the effects
of antidepressent medications. Schizophrenia.com members suggest fish
oil supplements (omega-3 fatty acids) or folate supplements. See
research supporting the use of nutritional supplements with medication.
- Many schizophrenia.com members say that a regular program of exercise
keeps them feeling mentally and physically healthy, and helps combat
negative symptoms such as depression and anhedonia. Numerous studies
have shown that exercise induces a positive physiological reaction
in the body (increases B-endorphins and monoamine neurotransmitters,
decreases stress hormones such as catecholamines). Moreover, exercise
gives a positive sense of accomplishment, an increased belief in oneself,
and positive benefits for physical health. Walking, exercise videos,
and yoga are good easy activities for a beginning exerciser, require
little/no equipment or training, and can be done either by yourself
or with a partner.
- For severe depression, talk with a doctor about electroconvulsive
therapy (shown to be safe and effective), or transcranial magnetic
stimulation.
Some online support groups and hotlines for you to try if you are feeling
depressed or suicidal:
1. American Suicide Survival Line (888) SUICIDE or, (888) 784-2433. This
nationwide suicide telephone hotline provides free 24-hour crisis counseling
for people who are suicidal or who are suffering the pain of depression.
2. The Samaritans Suicide Hotline (212) 673-3000.
3. Covenant House Nineline (800) 999-9999
http://www.covenanthouse.org
This hotline provides crisis intervention, support and referrals for
youth and adults in crisis, including those who are feeling depressed
and suicidal.
4. Internet site: http://www.metanoia.org/suicide/
For those contemplating suicide.
5. Internet site: http://www.save.org/index.html
This is the Web site for SAVE (Suicide Awareness Voices of Education),
whose mission is to educate others about suicide and to speak for suicide
survivors.
More resources to help yourself or a family member who's depressed:
What are the chances of relapse? How can you plan for a relapse situation?
Medication may be controlling symptoms and working well for a long
time; however, even a correctly dosed antipsychotic will not totally
guarantee against an eventual relapse. Most medications claim to reduce
chance of relapse by about 80%. Be aware that additional medications
might be needed to specifically address anxiety, depression, or panic
attacks.
Dr. E. Fuller Torrey in his book "Surviving Schizophrenia"
identifies common signs and symptoms (ironically, the symptoms were
largely the same whether reported by the patient or by families) preceding
a relapse episode. These can include: tenseness and nervousness (of
either the patient or the home environment in general), trouble concentrating,
depression, trouble sleeping, loss of interest in things/enjoying thins
less, being overly preoccupied with one or two things (Surviving
Schizophrenia, p. 289). Both patients and families will learn over
time what individual symptoms tend to herald a relapse.
The family and living environment is key to the recovery process. A
low-stress, low-key emotional environment can reduce the chances of
relapse. Patients and their families can be aware of what is a high-stress
situation or environment, and take steps to avoid those things. It's
a good idea to have a straightforward plan to implement in a "get
worse" case, as schizophrenia is a very unpredictable disorder
and will naturally have its ups and downs.. Keep resources - people
you can call on, emergency numbers, lists of medications, etc - close
at hand. See Tips
for Handling a Crisis and What
Relatives Can Do to Help Improve the Course of Illness.
Consider discussing the possibility of an Advance
Psychiatric Directive, to help guide family members and healthcare
professionals during a crisis.
How do I explain the illness to family, close friends, and others?
First, decide who you want to tell (family and close friends who will
be supportive and understanding, who might be involved in the recovery
process) and who you need to tell (doctors, school administrators, employers).
Not everyone needs to know, and for the most part you can be as discriminating
as you wish about how much you disclose.
Once you've decided to tell someone about the illness, be proactive
about providing information - books, articles, internet links - that
will help them understand. Know that some people will be sympathetic
and supportive, and some will not. Schizophrenia is a hard disease to
deal with and understand, and some people are just unable to empathize.
Some members of schizophrenia.com suggest distancing yourself, to a
degree, from relatives and friends who cannot seem to understand or
be helpful. It's important to you and your ill family member that you
both stay as positive and as hopeful as you can about the illness.
Our online PDF reference library contains
documents that are ideal for printing and passing out to family, friends,
and others who you would like to share information with about schizophrenia
and mental ilness-related issues.
Living with a Severe Mental Illness - Practical Matters:
As with any other chronic illness, there are some practical matters
that caregivers and other family members will need to eventually deal
with. These might include:
- insurance problems and driving licences
- befriending and leisure activities
- finding appropriate accommodation with any necessary support
- sheltered employment and training for work
- benefits problems and debts
- legal rights and advocacy
- genetic counselling
- treatment, including medication and complementary therapies
- representation at tribunal, court or inquest
Know that you have resources to help you plan these matters. For example:
- Treating psychiatrist or therapist
- social workers at the hospital
- local community organizations for the disabled
- PLAN
(Planned Lifetime Assistance Network): developed to meet the needs
of families who are actively planning for the future of an adult child
with a disability. Programs (currently available in 22 states) help
families develop a future-care plan, establish the resources for payment,
and identify the person(s) or program(s) responsible for carrying
out the plan. May also provide current services that relieve parents
of part of the daily burden of care.
- In the UK: Rethink,
the largest mental illness charity in the U.K., has information
relating to medical, legal and financial benefits available.
The following is a list of federal aid programs and funding to help
people with mental and physical disabilities. (Source: Mental
Health, Mental Illness, Healthy Aging, a guidebook from the New
Hampshire chapter of NAMI):
Disability Benefits (SSDI): Benefits exist for workers who become
physically or mentally disabled prior to retirement age. Disability
must be severe enough to prohibit substantial work and be expected to
last for a year or more. Generally provides a higher income than SSI.
Supplemental Security (SSI): Provides monthly cash payment to
aged, blind, and disabled people who have little or no income. Recipients
may be eligible for Medicaid benefits. A handicapped child under age
18 may receive this if the child and parent meet income and resource
requirements. Those eligible for SSI may also be eligible for benefits
such as housing programs, Medicaid, vocational rehabilitation, and food
stamps. Children living at home (in some states) can qualify for an
extra benefit under "living arrangements", which is meant
to offset some of the costs of providing extra attention and care to
a special-needs child living at home. NOTE: Many people are denied on
their first application, but are later accepted through an appeals process.
See NAMI's
page on Social Security Benefits, with a list of questions and answers
such as who is eligible, how to apply, and what to do if an application
is denied. . See also Help
With US Social Security Insurance.
National Council on Aging: The National Council on Aging (NCOA)
has a website designed to help older Americans determine what federal
and state benefits and programs are available, depending on the individual's
circumstances and request. The website can be accessed at www.benefitscheckup.org.
Aid to the Permanently and Totally Disabled (APTD): Provides
financial assistance to persons determined to be medically disabled
and meeting financial need guidelines. Income and other assets are considered.
Eligibility guidelines are based on financial need and disability rather
than age.
Some thoughts on applying for SSI or SSDI from schizophrenia.com members:
What SSI needs to see is letters from several professionals who
have worked with the person, which state that he/she has a severe
and permanent disability, that has a name (either medical or from
the psychiatry DSM-IV, the Diagnostic and Statistical Manual, 4th
edition), and that as a result of this disability she is unlikely
ever to be able to earn more than about $500 per month. Obviously,
to do this several things must be in place:
1) The ill person has seen a physician, psychiatrist, etc., been
examined, and found to meet criterion for such a diagnosis.
2) You must be able to communicate with the professional (with mental
illness this is next to impossible unless the ill person has filled
out a release of information form saying it's OK).
3) Tthe professional must agree to fill out the forms and write a
letter to SSI, and then actually do it.
Any person seeking SSI can have another person appointed to handle
all the paper work, etc. Be aware that the Social Security Administration
has a reputation for denying the first claim and the first appeal
(which is a paper review, that is almost always a rubber-stamped denial).
In seventy percent of secondary appeals, the decision is overturned,
and SSI is granted. The second appeal is heard in front of an Administrative
Law Judge, which in reality is not officially a "judge,"
but is a lawyer who specializes in administrative law. SSI will be
back-paid from the original application. A lawyer can really help
with this process, and many will take a percentage of the back SSI;
so there is no out-of-pocket cost.
The following are health insurance and aid programs for disabled or
low-income persons. (Source: Mental
Health, Mental Illness, Healthy Aging, a guidebook from the New
Hampshire chapter of NAMI):
Medicaid. Medicaid program helps pay for health care costs for
all persons who receive public assistance and for certain persons with
low incomes who can't afford the cost of health care. Criteria for this
program is the same as Aid to Persons Who Are Totally Dependent (APTD),
and persons receiving APTD may also qualify for Medicaid benefits. The
Old Age Assistance (OAA) program applies to individuals who are 65 years
and older.
Medicare: This federal health insurance program offers hospital
insurance coverage (Part A) and medical insurance (Part B) for people
65 and older who qualify for retirement benefits, for workers who have
been receiving disability benefits for 24 months or more, and for people
who need kidney and dialysis or transplant. There are various plans,
with some mental health benefits included. To apply, call 1-800-772-1213.
QMB/SLMB: This provision pays the portion of Medicare that covers
health insurance. Check with your local Division of Health and Human
Services office for more information.
HICEAS: This program provides health insurance counseling, education,
and assistance services to assist Medicare beneficiaries and their families
in understanding their insurance coverage and options. For more information:
1-800-852-3388.
Home Health Care: These are in home medical services for qualified
older adults in their home. Local visiting nurse or home health associations
usually provide home health care. Medicare may cover certain medical
and psychiatric services.
Lifeline: This is a personal response service for persons if
they fall or have an emergency. It involves using a machine and a help
button that calls a central number and is available for a monthly fee.
For more information call: 1-800-635-6156.
For more information, see "Mental
Health Insurance" news and information.
Housing concerns - if your loved one can't live at home:
Often, a mentally ill family member is unable to be self-sufficient
and completely independent, even if they are of legal age to be living
alone. In these situations, other arrangements can be made, either in
the home or in another facility.
Many families are neither prepared nor equipped to accept a mentally
ill relative into their homes, particularly if they have a job and a
family of their own. It's most important that the patient be on medication,
and if you have no way to ensure that in your house, then taking them
in helps no one. Moreover, psychotic episodes may put you or your children
in danger. Experts suggest that having a mentally ill family member
live with you may work under the following circumstances:
o the ill person functions at a fairly high level, has friendships,
and is involved in activities outside the house
o if there are young children, their lives are not negatively affected
o interaction among family members is relaxed, and
o the ill person intends to take advantage of available support services
However, under other circumstances (see below), another arrangement
might be more appropriate:
o the main support person is single, ill, or elderly
o the person with schizophrenia is so seriously ill that there is
little
or no chance to lead a normal family life
o children become frightened and resentful, and feel like they are
living in a hospital
o marital relationships deteriorate
o most family concerns revolve around the person with schizophrenia
o no support services are used, or services are not available
o the individual is habitually aggressive, and the threat of violence
disturbs the household.
Even though you may feel obligated to help your family member, and guilty
about not taking on the responsibility, you first have an obligation
to yourself (your own mental and physical health and well-being) and
your family. The best thing for everyone involved is to find them another,
supportive place to live. Research treatment centers, halfway houses,
group homes, crisis housing, clubhouses, or a live-in home/nursing aide.
The following is a list of housing options for the mentally ill, as
well as federal/charitable support and aid programs (Source: Mental
Health, Mental Illness, Healthy Aging, a guidebook from the New
Hampshire chapter of NAMI):
Independent Living: in a subsidized apartment or using federal
aid for rent
Supervised apartment: You may have your own apartment, or share
an apartment with one or two other clients. Staff members are on call
to assist you, and they stop by routinely to see how you're doing.
Home-share: You may share a home with several other clients.
Your case manager visits you at your home and assists you if you need
help with anything.
Foster care: You may live with a family that has received training
and support in providing a place to live for a person who has a mental
illness disability.
Community care home (group home): This type of group living
arrangement serves only people with mental illness disabilities. Professionals
and trained staff are available on the premises to assist you.
Halfway house (group home): This arrangement is particularly
helpful for a patient with a dual diagnosis of addiction and mental
illness. Professionals at the halfway house offer help to the resident
needing assistance with this type of dual recovery.
Boarding home (group home): You may share a home with other
clients, and people are available to assist you. This type of housing
is different from a "community care home"; the people who
are available to assist you are not mental health care professionals.
However, they have received training to assist people with mental illnesses.
Clubhouse: The participants are called members, not patients
and the focus is on their strengths not their illness. Work in the clubhouse,
whether it is clerical, data input, meal preparation or reaching out
to their fellow members, provides the core healing process. One of the
most important steps members take toward greater independence is transitional
employment, where they work in the community at real jobs. Members also
receive help in securing housing, advancing their education obtaining
good psychiatric and medical care and maintaining government benefits.
Membership is for life so members have all the time they need to secure
their new life in the community.
Residential treatment facility (group home): This is another
type of group living arrangement that treats people with disabilities
caused by mental illnesses. A large staff of professionals is available,
and people usually stay in this type of facility for long periods of
time. Clients attend classes or workshops to learn skills to become
more independent.
Temporary respite bed: This temporary living arrangement is
available for people having a crisis. Staff members are available to
help clients through the crisis period.
Nursing home: This type of facility offers 24-hour care and
is staffed by physical and mental health professionals. The client using
this type of service is generally the elderly mental health patient
Resource links to housing and aid programs:
1) Mental Health America's list of Federal
programs providing housing aid for people with disabilities to live
independently in the community.
2) The Fountain
House is the original Clubhouse for the mentally ill, founded in
New York and now with 250 centers in 43 states. Fountain House has programs
for housing, education, outreach, advocacy, and social/recreational
activities.
3) International
directory of clubhouses.
4) Your local NAMI
chapter or support group may have some useful resources in your
area. Look also to see if there is an Assertive
Community Treatment program in your area
5)Contact local Public Housing Authorities (you can find them listed
under county/city offices in the gov pages of the phone book - may not
be under exactly that name) - they are responsible for allocating Federal
funds for low-cost and subsidized housing. They will know what is available
in your area.
Schizophrenia.com members who have gone through the experience of finding
appropriate housing for an ill loved one recommend finding a support
group or a counselor to talk over your options and your own emotions
about the situation. It's a terribly draining experience, and speaking
to others who have had to deal with similar situations can be an excellent
support.
Job and School Issues - can a person with schizophrenia
go back to work? Should they?
Like so many questions about schizophrenia, the short answer to the
employment question is "yes and no." Since there is such a
wide spectrum of severity under the schizophrenia diagnosis, some people
will eventually be able to go back to work full-time, others can take
a part-time job with accommodations, still others can find satisfaction
in volunteer work, and some simply don't have the capacity to do any
of the above. A good predictors for future employment (according to
Dr. E. Fuller Torrey, "Surviving Schizophrenia") is if the
person held a job before becoming ill. If they have held a job in the
past, it is more likely they will be able to hold a job sometime in
the future. Likewise for pursuing a higher education degree, much depends
on the individual situation. Someone who has their symptoms under good
control, and is effectively managing their illness, may be ready to
take on the added stress (but also the added rewards) of higher education.
There are always some pros and cons to consider. Pros include increased
self-esteem, a reason to get up in the morning, a positive identity,
an extended social network, and additional income (although check to
see how working will affect federal benefits, if applicable).
Cons include possible stigma in the workplace, symptoms of illness or
side-effects of medication (i.e. fatigue, difficulty concentrating,
distraction) make working hard or impossible, added stress of a job
contributing to relapse, and possibility of losing social security or
other healthcare benefits. According to the Social
Security Association website, returning to work does not automatically
disqualify a person from disability benefits. Familiarize yourself with
the legislation, frequently asked questions, and support programs using
the following information resources:
If you've decided that returning to work is possible and desirable,
think about the kind of work you have the skills to do (or could learn
the skills to do), and that you would potentially enjoy. The cognitive
symptoms of the illness (distractibility, fatigue, social withdrawal,
inability to concentrate, etc) may limit what you can aspire to do,
but there are still jobs out there. Know the things that stress you
out in day-to-day living, and take those into account. Maybe look for
something that requires minimal social interaction, or a job you could
do from home.
Making the transition into work (either full-time or part-time) can
be difficult, as you are rehabilitating from a long illness episode.
The following suggestions from board members may help you work up stamina
and gauge your own abilities before attempting to take a formal job:
- Volunteer (this can help you acquire skills, build up contacts,
and it looks good on the resume. It can be very enjoyable as well!)
- Take a class at the local college, or sign up for correspondence
learning courses. Some schizophrenia.com members are currently working
on, or have recently finished, college-level degrees. See the "work
and school" board - a subconference under 'People Diagnosed With
Schiz' to read their posts and ask your own questions.
- Attend church functions (bible study, church picnics, forums, etc.)
- Start your own business
- Get out and exercise
Some schizophrenia.com members have posted on the boards that they
feel overwhelmed at work or school, and have trouble managing deadlines,
prioritizing tasks, and keeping focused. If you are currently struggling
at work, here are some suggestions that may help. (Note: some are suggestions
from schizophrenia.com members, some are excerpted from "Diagnosis:
Schizophrenia" by Rachel Miller and Susan E. Mason).
1. Talk to your doctor or a social services agency about finding
a job coach (this is something specific mentioned by several people
on the Discussion Boards) that can help you with your specific work-related
problems and be a supportive voice.
2. Keep lists of small goals and deadlines, number them according
to which need to be done first, and look at the list every morning
and evening. Check things off when they get done, and revel in the
satisfaction.
3. Keep a calendar or a day planner where you can immediately write
down all appointments, tasks, and reminders for yourself
4. Make a list of short-and long-term goals, broken down into manageable
steps. A job coach, a social worker, or a supportive friend or family
member can help with this.
5. Keep your work environment as noise- and distraction-free as possible.
6. If possible, work for short periods of time separated by breaks.
For either work situations or higher education, the following tips
might be helpful:
- Know your support resources. Find out about on-campus
counseling and disability services ahead of time. Know what support
services will be available to you as someone with a mental illness
diagnosis. Register with your school's office of disabilities.
- Know your rights. You are not required by law to
disclose a mental illness diagnosis to your employer. Consider the
relative pros and cons of sharing this information - the benefits
of added support, understanding, and accommodations, vs. the possibility
of stigma and discrimination.
- Present your needs. Know what sort of accommodations
you might need to help you succeed under the stress of work or school,
and discuss them with your employer and/or the school disability office.
Will you need flexible, part-time work? A note-taking or transcribing
service? Extra sick days? A partner for training or moral support?
Identify your needs, and present them calmly and clearly.
Other resources to help you in returning to work:
How Can I Help a Family Member Who's Been Arrested?
This is, tragically, not that uncommon a concern for families of schizophrenia
patients. It's important to know that people with schizophrenia are
not more violent than the average person - as long as they are receiving
adequate treatment. However, it is increasingly difficult for people
with schizophrenia to get and stay in treatment, and this is perhaps
why about 1 in 6 inmates have some sort of mental illness.
Once someone has been arrested, they are in the domain of the legal
system, which can be just as if not more confusing than the medical
system. Right now there is not very good coordination between these
two systems to help offenders with brain disease. However, there are
some things that you can do, and some resources you can tap.
The following suggestions have been adapted for general use from NAMI
publications by the chapters
of California and Wisconsin.
Depending on your state regulations, these may or may not work for you.
Look up your local Protection
and Advocacy Agency, which offers services for mentally ill citizens,
and ask for legal advice pertaining to your area.:
1) Offer your support. Help your loved one stay calm, and remind him/her
of legal rights (right to an attorney, etc).
2) Contact the local jail where your relative is being held. Let the
offical in charge know that your relative has a psychiatric disorder,
and give information about the specific diagnosis and symptoms. Ask
how long your loved one is expected to be held. and ask the jail staff
about arranging a psychiatric evaluation. If he/she is seriously ill,
you can ask for a police transport to a psychiatric hospital (this is
called a "5150" hold) for three days of evaluation and treatment.
Ask about the possibility of receiving medication at the holding facility
(it seems like medication is generally available only at County jails,
not city ones).
3) Notify your loved one's psychiatrist, case manager, and the jail
medical staff or administrator of the situation, and stress the importance
of continuing uninterrupted medical care.
3) If and when your relative is transferred to a county jail facility,
contact them and ask for their location and booking number. Ask if you
can fax over information regarding your relative's medical diagnosis,
and ask about placement in a mental health unit (if available). Information
to be included: diagnosis, psychiatrist's name/phone/address, medical
doctor's name/phone/address, medications with dosages and times to be
administered, side effects that your loved one experiences, history
of suicide threats/attempts, other medical conditions and medications
prescribed for them. Providing this information can help the staff in
conducting their own assessment before placing your loved one in a mental
health unit. Keep the information in the fax medically-related only,
and keep a copy for future reference.
4) Find out if there are any Mental
Health Courts in your area - these are special courts that assist
mentally ill offenders. Sometimes these courts make decisions to release
an offender (after a certain portion of the sentence is served) on the
condition that the person remain in an approved treatment program.
5) Decide about legal representation. If you do not have a private
attorney, your loved one will be assigned a public defender. Don't automatically
assume that the public defender will do a less credible job than a private
one; do some research and find out about all options. A local support
group such as a NAMI chapter might be a good resource for this, if other
families have had experience in the local legal system. Also, see the
American Bar Association's Disability
Lawyers Directory.
6) Resources you can contact for assistance:
--The National Association
of Protection and Advocacy Systems
--The Bazelon Center
for Mental Health Laws (202-467-5730)
--The Treatment Advocacy
Center (703-294-6001).
--The Consensus
Project - a national effort to improve the services to people with
mental illness in the criminal justice system.
An excellent book on this subject is "Northumberland
Nightmare", written by a father whose mentally ill son was
charged and incarcerated for robbing a bank. He writes about difficult
encounters with both the legal and medical system in the struggle to
get fair and decent treatment for his son.
Listen online to two public radio special reports on the situation
of the mentally ill in America's jails:
--Jailing the Mentally Ill: A Two
Part Special Report
--The Concept of Legal Insanity
|
|



