|
Common Questions from People who's Parents have schizophrenia
The following are questions commonly posted on our discussion boards,
along with answers and advice from responding members. In many cases,
member answers have been expanded on from other sources, and relevant
links have been addedfor more information. These answers are meant only
as a helpful guide and a resource for further information; each individual
situation is unique and may need a tailored solution. Your relative's
treating psychiatrist is always a good person to ask when you have specific
questions pertaining to your own case.
If you don't find what you're looking for here, please visit the Schizophrenia
Offspring Discussion Board (see the righthand menu column on the Schizophrenia.com
homepage ) and post your question. Our members are usually very generous
with their advice and support. The questions in this FAQ section are geared
mainly towards older teenage and adult offspring; however, there is a
special subsection in the Offspring Discussion Boards for adolescents.
Index of Questions
My mother/father is becoming more paranoid and acting
odd - is this schizophrenia? Could it be something else?
What are my chances of inheriting schizophrenia from
my parent? What are the chances that I could pass it on to my own children?
Do children of parents with schizophrenia have a higher
incidence of other, related psychiatric conditions?
What common issues/concerns do children of parents
with schizophrenia deal with, and how do they cope?
I am a student/I have a full-time job/I live far
away. How can I make sure my parent is taking care of themselves?
What if my parent wants to come live with me?
Deciding to obtain guardianship or power of attorney
Is my parent eligible for disability aid or health insurance?
How can I help a parent (or older family member)
who's depressed?
Living with a mentally ill parent is affecting my
own thoughts - I have to remind myself who's delusional! Is this common?
How do I explain to my children about Grandma/Grandpa's
illness? Should I keep them from visiting?
My mother/father is becoming more paranoid and acting odd - is this
schizophrenia? Could it be something else?
Depending on your parent's age, odd, paranoid, or even psychotic behavior
could be a sign of a type of dementia. According to Geriatric Consultant
Resources, psychotic
or behavioral disturbances in the elderly population is most often associated
with dementia, with Alzheimer's disease accounting for more than
60% of psychotic symptoms in the elderly. Normally, schizophrenia is
diagnosed when the patient is in their late teens or twenties. Late-onset
schizophrenia (diagnosis after age 40 or so) is more uncommon, and seems
to be slightly more predominant in females of this age group. Research
indicates that out of all patients hospitalized for schizophrenia, 13%
have onset of symptoms in their 50s, 7% in their 60s, and 3% in their
70s or later.
For specific information on late-onset schizophrenia and other forms
of dementia/psychosis, see the following online audio/video presentations:
1. Schizophrenia
and Aging (NPR)
2. Schizophrenia
in Late Life: What is New and What is Old? (UCLA grand rounds)
3. Schizophrenia
and Aging: Myths and Reality (U. Chicago grand rounds)
See the General FAQ guide - symptoms and
diagosis section for more information on how schizophrenia is recognized
and diagnosed. However, regardless of the cause, symptoms that are debilitating
to the person should be evaluated. Talk
to a doctor, explain the situation and the symptoms ahead of time,
and encourage your parent to make an appointment. If your parent doesn't
want to see a doctor (a common problem for family members of the mentally
ill) and you are still concerned about their behavior, see 'What
if my family member refuses to see a doctor' for ideas.
If you do eventually receive a diagnosis of schizophrenia, see 'What
to do after receiving a diagnosis - how you can help' for ideas
and support.
What are my chances of inheriting schizophrenia
from my parent? What are the chances that I could pass it on to my own
children? What are my risks of getting schizophrenia if a family member
or relative has schizophrenia?
As author Victoria Secunda points out by quoting the following "High-Risk"
study in her book When Madness Comes Home, "...an individual's
chances of succumbing to psychopathology or maladjustment are influenced
by the patterns of the individual's life...The fact that someone
has a schizophrenic parent implies nothing necessarily about that individual
beyond the fact that he or she has a schizophrenic parent." (p.
209). While this may be true, it is also true that Population
statistics on the heredity of schizophrenia estimate that a child
with one diagnosed parent has about a 10% genetic risk of developing
the disease themselves (this is compared to a 1% risk in the general
population). The risk goes up significantly if a grandparent (or other
close relatives) also has schizophrenia. (E.F. Torry, 1996).
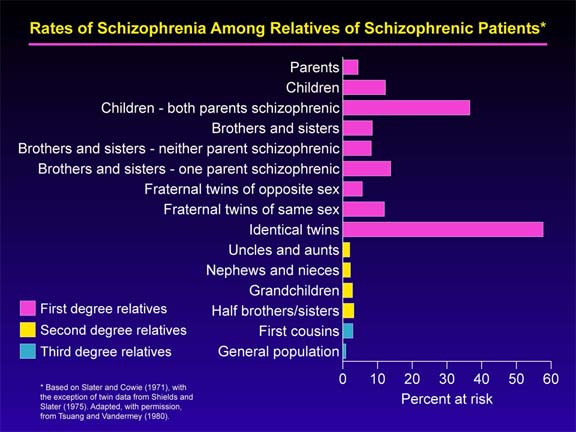
(Image Source: Debby Tsuang, M.D., M.Sc., University of Washington/VAPSHCS, Special thanks to Dr. Kristin Cadenhead, UCSD)
Genetic inheritance is only one of the many factors (both biological
and environmental) that contribute to the cause of schizophrenia. Moreover,
research indicates that the inheritance of such a complex disorder likely
involves a number of genes, some of which we may not know about
yet. You may have inherited an increased predisposition to schizophrenia
(or a related disorder) from your parent; however, not everyone who
carries such a predisposition will develop the symptoms. In many cases,
living in what is considered a "low-risk" environment for
developing mental health problems is protective for those with either
high orlow genetic risk.
For more information on the genetics of schizophrenia, as well as the
environmental factors involved with schizophrenia and the steps you
can take to lower your own and your children's risk of developing schizophrenia
or another psychiatric disorder, see Causes
of schizophrenia and Schizophrenia Prevention Strategies.
Do children of parents with schizophrenia have
a higher incidence of other, related psychiatric conditions?
Since schizophrenia seems to involve
multiple genes, it's certainly possible to inherit only some of
them and be affected in a different way. Other conditions such as depression,
panic disorder, Asperger's or Autism, or even extraordinarily low self
esteem seem to be common among children of parents with schizophrenia.
This could be related to genetic inheritance, the general stress of
being a primary caregiver to a mentally ill parent, or a combination
of factors.
Some children also exhibit symptoms of Post Traumatic Stress Disorder
(PTSD), the result of, as one schizophrenia.com member put it, "growing
up in a war zone with no training, no army behind us, [and] no rules."
It's very important for children of mentally ill parents, whether they
are formally diagnosed with a disorder or not, to get support for their
own difficult situations. Many children of schizophrenic parents on
our boards have indicated that support
groups or individual
therapy has been extremely important in their own lives. Learn more about Schizophrenia Prevention Strategies.
What common issues/concerns do children of
parents with schizophrenia deal with, and how do they cope?
All of these children, whether young or old, naturally have strong
feelings surrounding their parent, their childhood, and the disease,
that affect them in a variety of ways throughout their own lives. Many
will choose (or have chosen) various defense mechanisms to help them
cope with their unique situations, including self-involvment (i.e. self
blame), dispacing anger or grief, denial, and defensive exclusion (emotional
detachment or distancing). These protective efforts can eventually lead
to long-term emotional patterns such as "anxious and ambivalent"
attachments, "compulsive caregiving," or avoidance of all
"affectional ties." (paraphrased from When Madness Comes
Home by Victoria Secunda, p. 52).
Some of the common issues raised by offspring on our discussion boards
include:
1. Boundaries: When you grow up with a parent who invades every aspect
of your life in unpredictable and sometimes dangerous ways, you can't
learn when to say no, when to back off of other people, etc.
2. Loyalty issues: Often times, especially when the parent is paranoid,
the kid is repeatedly put in a situation where they need to "prove"
that they aren't part of the "bad guys." This is part of the
boundary issue - It's a tricky thing, trying to keep your sanity while
trying to placate an insane person when you're a kid.
3. Social skills: A lot of us on this board have some difficulty once
we hit adulthood with knowing who and how to open up to people, or how
to trust our instincts about situations, and in general, how to negotiate
around "normal" people. [We] were shut off from the rest of
the world because of our parents, both physically and psychologically.
4. Life skills: If kids are still living with their ill parent, they
often won't learn basic skills such as how to clean a house, cook, or
pay bills..
5. Anger/Depression/Stress management: We offspring are often very
depressed well into adulthood. Many have personal counselors/therapists,
are involved in a peer counseling support group, or take medication
for depressive, anxiety/mood disorders.
6. Guilt management: [Offspring] are especially prone to feeling a
lot of guilt about everything. Many go through a phase of blaming themselves
for the parent's illness. Almost all feel guilty for not doing enough
(or doing too much) for the parent, other siblings, or the rest of the
family.
7. Fear: Fear of becoming like the ill parent, or fear of becoming
ill themselves has actually changed the trajectory of many children's
lives. They delay having children for fear of "passing it on."
They delay marriage because of not wanting kids, or not wanting to hurt
a loved one by becoming mentally ill in the future. Often these children
deal with a huge amount of self-criticism.
8. Attachment issues: may avoid attachments, or may become involved
in overly-needy or abusive attachments.
9. Forgiveness: is often confused with acceptance. Acceptance of a
parent's mental illness is an important step for self-healing and recovery;
however, it is not required that you forgive your parent to reach
that acceptance.
According to author Victoria Secunda, the offspring of mentally ill
parents fare the best when they have several sources of support:
supportive relationships with a well parent, relative, or friend, support
from mental health care systems and professionals, and support from
the legal system. "The hope...rests on the ability of well members
of the family, in partnership with outside resources, to both
contain the damage of a sever brain disturbance and to prevent the conditions
that might evoke it in the next generation." (Secunda, When
Madness Comes Home, p. 62).
Depending on your personal situation and/or feelings, you may or may
not want to stay in contact with your parent after you become independent.
That decision must be made by you and for your own best interests; however,
counseling or support
groups may help you deal with some inevitable guilt, frustration,
or uncertainty about the decision. Author Victoria Secunda indicates
that 79% percent of offspring and 74% of siblings of mentally ill patients
out of those she interviewed for her book were or had been been in therapy.
"Virtually all of them say that it has transformed them. Through
therapy, they have restored their faith in themselves and in others,
and have regained a sense of control over their lives." (Secunda,
When Madness Comes Home, p. 282).
Schizophrenia.com has many excellent
books, both reference and memoirs, for family members of schizophrenia
patients. These books come recommended by others who have firsthand
experience in dealing with mental illness. We also have links to over
a 100 different internet -based videos and audio files - some of
which deal with these issues.
I am a student/I have a full-time job/I
live far away. How can I make sure my parent is taking care of themselves?
This is a concern that many adult offspring face as they start lives
and families of their own, and their ill parent is still unable to be
completely independent. The situation - and the solution - will be different
depending on if your parent is in treatment, is medication-compliant,
is living independently or in a group home/treatment center, is financially
independent, etc. The following are some solutions used by members of
schizophrenia.com to deal with their own situations - they may be helpful
to you, or you may find a resource for advice/information.
1) If your parent is living independently and you are concerned for
them, look into hiring a part-time home aid. Such a person can come
to your parent's house for a few hours every day to check in, make sure
medications are taken, help with errands and around the house, and just
generally visit. Your parent's insurance may cover home help.
2) If you have other siblings or your parent has close family still
living, try and share the responsibility with a larger group of people.
Everyone pitching in a little goes a long ways, and someone might live
closer or be better equipped to give care than you are right now.
3) Explore ways to simplify your parent's treatment regimen, such as
using compartamentalized pill containers, automated pill-notification
systems, or switching to long-acting injectable medications. Many schizophrenia
patients are far more able to care for themselves and live independently
if they consistently take their medication. If you're concerned that
your parent is refusing to take their medication or cooperate with their
treatment, see the General FAQ section
on treatment issues for ideas.
4) Appoint a lawyer or another conservator to handle finances and make
sure the bills are paid.
5) Contact a local
support group or mental health center, and ask what resources are
available in your parent's area.
What if my parent wants to come live with me?
Even though many children feel obligated to help their ill parent
or guilty about not taking on the responsibility, most are neither prepared
nor equipped to accept a mentally ill parent into their homes, particularly
if they have a job and a family of their own. It's most important that
the patient stay in treatment, and if you cannot ensure that in your
house, then taking them in helps no one. Your first obligation must
be to yourself (your own mental and physical health and well-being)
and to your children, if you have any.
In many situations, the best thing for everyone involved is to find
the ill parent another place to live. Research treatment centers, halfway
houses, group homes, or a live-in home/nursing aide. Below are some
resources to get you started:
1) National Mental Health Association's list of Federal
programs providing housing aid for people with disabilities to live
independently in the community.
2) The Fountain
House is the original Clubhouse for the mentally ill, founded in
New York and now with 250 centers in 43 states. Fountain House has programs
for housing, education, outreach, advocacy, and social/recreational
activities.
3) International
directory of clubhouses.
4) Your local NAMI
chapter or support group may have some useful resources in your
area. Look also to see if there is an Assertive
Community Treatment program in your area
5)Contact local Public Housing Authorities (you can find them listed
under county/city offices in the gov pages of the phone book - may not
be under exactly that name) - they are responsible for allocating Federal
funds for low-cost and subsidized housing. They will know what is available
in your area.
See General FAQ - housing concerns
for a further description of what options are available.
Schizophrenia.com members who have gone through the experience of finding
appropriate housing for an ill loved one recommend finding a support
group or a counselor to talk over your options and your own emotions
about the situation. It's a terribly draining experience, and speaking
to others who have had to deal with similar situations can be an excellent
support.
Deciding to obtain guardianship or power of
attorney:
If the illness is severely debilitating, some children consider obtaining
guardianship, conservatorship, or power of attorney over their mother
or father. Depending on what kind of legal standing you obtain, it can
assign you the right to manage your parent's financial affairs and assets,
and/or make treatment decisions on their behalf. Below are descriptions
of the different types of legal guardianship one can have over a disabled
adult:
Guardianship: May be considered in situations where an individual
becomes incapacitated due to their mental or physical condition. In
situations where an individual has become so incapacitated and unable
to make sound decisions that they are facing either a prolonged or serious
risk, it may be necessary to consider seeking guardianship. Persons
must prove that they cannot care for themselves and need someone to
look after their best interest. The process is extensive and requires
the approval of a court. Guardianship is an involuntary protection imposed
by the probate court only when necessary to protect a vulnerable person
from harm, and only when other options such as a power of attorney or
representative payeeship are not possible.
Durable Power of Attorney for Health Care: Allows the older
adult to direct whether or not life sustaining treatment should be given;
also allows the older adult to name a trusted person (agent) to make
medical decisions.
Financial Power of Attorney: Allows an adult to appoint someone
they trust to pay bills; cash or deposit checks; deal with insurance;
take care of other financial matters as needed. It is highly recommended
that people see an attorney for this process. State law requires specific
language in order for the power of attorney to be legally effective.
Representative Payeeship: A representative payee can be assigned
to manage social security benefits on behalf of an individual if he/she
is unable to manage the monthly check. A payee can be an identified
family member or caregiver. A document must be filed with the Social
Security Administration that states why the person needs a representative
payee. This is an involuntary process imposed by Social Security when
necessary to protect the recipient. Social Security will decide based
on medical information whether payeeship is necessary.
Be aware that guardianship, depending on your state and situation,
may or may not give you the what you're looking for; in other words,
it may make your situation harder instead of easier. It gives you legal
and financial power, but does not really give you any more control over
your parent than you ever had. As one schizophrenia.com member put it,
"I have never found a way to force an adult to do anything they
don't want to do, even with rational adults, And schizophrenics are
not rational." You might be setting yourself up for a long haul
of frustration and burden. See Assisted treatment
options for ideas on what to do if your parent is not treatment
compliant - there are other things to try before obtaining the lifelong
post of legal guardian.
An Advanced Psychiatric Directive is also an option to discuss during
times when the ill person is in control and in a reasonable frame of
mind. This legal document allows the person with the illness to dictate
what actions should be taken on their behalf (including appointing another
person to make treatment decisions) if they should become unable to
make decisions for their own well-being. Bear in mind that Advance Directives
are not appropriate for all, or maybe even the majority, of people with
schizophrenia. In order for a Directive to be an empowering rather than
a coercive tool, the person who prepares the document for themselves
must have the skills and the social support to make beneficial decisions.
For more information, and for downloadable documents to help prepare
an AD, see the Advanced
Psychiatric Directives section of the Bazelon Mental Health Law
Website.
If you decide that obtaining legal power over your parent is the best
course of action, check with the psychiatrist and/or social workers
at the hospital to find out what the procedure in your area is, or look
up individual state laws online.
Is my parent eligible for disability aid or health
insurance?
See General FAQ - Practical Matters
for a description of available federal funding, aid, and health insurance
programs for the disabled, the low-income, or the elderly. (Source:
Mental
Health, Mental Illness, Healthy Aging, a guidebook from the New
Hampshire chapter of NAMI)
How can I help a parent (or older family member)
who's depressed?
Depression is not uncommon in the elderly, particularly those who have
outlived many of their family and friends, or who have moved away from
their homes or familiar places. Schizophrenia patients may be especially
likely to suffer from depression. Many take antidepressants along with
antipsychotic medication, or attend additional counseling/support groups,
to help manage these symptoms.
NAMI recommends the following steps to help the elderly with depression.
You can help your family member:
- Maintain spiritual customs, social customs, old relationships, and
family connections
- Develop new relationships (through clubs, church functions, nursing
home, senior day centers, etc)
- Tend to grandchildren or other young children in the family
- Explore civic and community activities (clubs, community centers,
day programs, churches, etc)
- Volunteer in the community (this is especially helpful for a lot
of schizophrenia patients; it is a good use of special skills or talents,
and keeps them feeling active and productive).
See Managing Depression
on the schizophrenia.com website for more information on recognizing
and coping with depression.
Living with a mentally ill parent is affecting
my own thoughts - I have to remind myself who's delusional! Is this common?
Many children living with schizophrenic parents do find themselves
"questioning their own sanity", largely because the paranoia
and hallucinations of the parent are so integrated into their normal
daily life. This does NOT necessarily mean that you have schizophrenia
(see 'How Can I Tell If Someone Has Schizophrenia'),
especially if you are able to distinguish between the real thoughts
and the delusional ones.
Talking to a therapist, counselor, or peer
support group can give you a good reality check, and relieve some
of your daily stress burden. It's important for someone to care for
the caregiver.
How do I explain to my children about Grandma/Grandpa's
illness? Should I keep them from visiting?
Your individual decision will depend on whether you still have contact
with your parent, and if you do, how severe their symptoms are. If you
decide to tell your child, base the amount you share on his/her maturity,
stability, and ability to understand. Answer any questions they have
as honestly as you can.
There are a few books about mental illness that are written specifically
for children. View
these books and their reviews at www.schizophrenia.com/media/.
Making a decision about visiting is something that most every adult
who has a relative with schizophrenia must face, and it's a hard one
for all of them. Many on the schizophrenia.com discussion boards have
made the decision that their own children and family comes first, and
have cut off communication with the ill relative to protect the children
from unnecessary emotional or physical harm. Some families bring their
children for very short, very supervised visits once they are older
and can understand why the illness makes people act the way they do.
Here are some sentences to open a discussion with your children. They
are based off of things that children of schizophrenic parents on our
discussion boards wish someone had told them.
"Your [grandmother/grandfather] has an illness called schizophrenia.
It makes it hard for her/him to think straight, and so they act very
oddly sometimes [examples of times the child has experienced or heard
about]."
"Remember that what you're seeing is symptoms of an illness. We're
all doing our best to help her/him get well, but this is a very serious
illness and hard to treat.
"Right now there is no cure for this illness. We really really
really hope there will be a cure someday, but right now there is none."
|



